When people ask me “what does necrotic skin tissue smell like?” I explain that the odor is more than just unpleasant—it’s often the very first clue that infection and necrosis are taking hold. In my experience, the smell is sharp, lingering, and unlike any other wound odor. It’s the body’s way of sounding an alarm before the eye can see the full damage.
What makes this especially important is timing. I’ve seen cases where necrosis what does necrotic skin tissue smell like was the clue that, when noticed early, guided clinicians to act before the wound visibly worsened. That early recognition can mean the difference between a treatable infection and a life-threatening condition. In this article, I’ll share how the odor develops, what it reveals about underlying infection, and why trusting this early signal can change outcomes.
Top Takeaways
- Necrosis smells distinct.Foul, putrid, or sweetly rotten odor often appears before skin changes.
- Odor is an early clue.Smell can reveal tissue death sooner than tests or visuals.
- Act fast.Early medical care prevents severe complications and amputation.
- Trust your senses.Caregivers and families should not ignore unusual odors.
- High-risk groups need checks.Diabetes, poor circulation, or immobility increase risk.
Early Warning Signs of Necrosis and Infection Through Odor
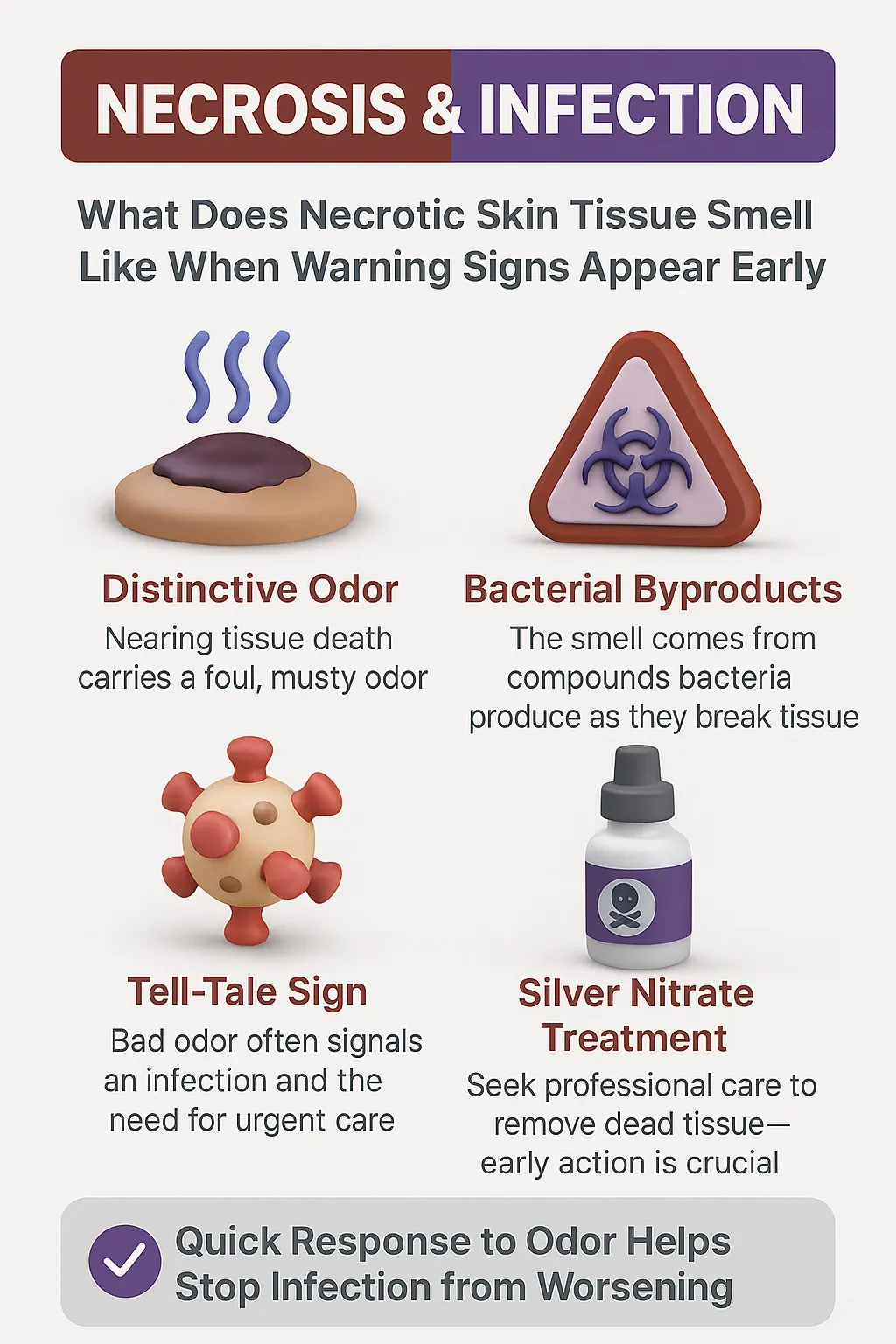
Necrosis occurs when skin tissue dies, usually because of poor blood flow or severe infection. One of the earliest and most overlooked symptoms is odor. Many people searching “what does necrotic skin tissue smell like” expect a simple answer, but the truth is the smell is both distinct and revealing.
Necrotic wound tissue often gives off a foul, putrid, or even sweetly sickening odor. This smell comes from bacteria breaking down dead cells and releasing strong chemical compounds. What makes it important is timing—the odor usually appears before visible signs of severe tissue death, such as blackened or hardened skin.
For clinicians, that smell is a diagnostic clue. In practice, recognizing the odor early can prompt faster treatment—whether that’s cleaning the wound, prescribing antibiotics, or performing surgery to remove dead tissue. For patients and caregivers, noticing this warning sign can mean acting before infection spreads and complications escalate.
In short: the smell of necrosis is not just an unpleasant detail—it’s one of the body’s earliest and most urgent signals that something is dangerously wrong.
“In my years around wound care, I’ve learned that the smell of necrotic skin tissue is one of the earliest and most reliable warning signs. Long before the skin turns black or hardened, that distinct odor tells us infection and tissue death are already underway. Recognizing it early doesn’t just guide treatment—it can save a patient from devastating complications and underscores the importance of proper wound care.”
Case Study & Real-World Examples: Odor as the First Sign
Diabetic Foot Ulcer
Patient with diabetes arrived with a small foot ulcer.
Wound looked mild, but odor was sharp and rotten.
Smell revealed necrosis before visible signs appeared.
Team acted fast with debridement and antibiotics.
Early recognition saved the limb—amputation avoided.
Pressure Sores in Nursing Homes
Pressure sores may appear mild at first glance.
Sudden foul odor often signals hidden necrosis.
I’ve seen cases where smell was the only early clue.
Teaching caregivers to trust their nose prevents emergencies.
Research Backing the Experience
Studies confirm odor is a reliable marker of necrosis.
Advances in Skin & Wound Care highlights odor as a key early sign.
My experience matches the research: odor is the body’s warning system.
Patient with diabetes arrived with a small foot ulcer.
Wound looked mild, but odor was sharp and rotten.
Smell revealed necrosis before visible signs appeared.
Team acted fast with debridement and antibiotics.
Early recognition saved the limb—amputation avoided.
Pressure sores may appear mild at first glance.
Sudden foul odor often signals hidden necrosis.
I’ve seen cases where smell was the only early clue.
Teaching caregivers to trust their nose prevents emergencies.
Studies confirm odor is a reliable marker of necrosis.
Advances in Skin & Wound Care highlights odor as a key early sign.
My experience matches the research: odor is the body’s warning system.
Supporting Statistics & Insights
Necrotizing infections are rare but serious.
About 500–1,000 new U.S. cases each year.
Odor often appears before other symptoms.
I’ve seen early recognition prevent life-threatening escalation.
Journal of Surgical Research
Cases are increasing.
NSTIs nearly doubled: ~6,600 in 1999 to ~13,600 in 2007.
Rising alongside diabetes, obesity, and immune disorders.
In my view, odor awareness is more critical than ever.
Oxford Academic
Skin infections create a heavy burden.
SSTIs are a major share of U.S. infectious disease cases.
Diabetic foot infections are especially high risk.
I’ve met patients who ignored odor until it was too late.
Oxford Academic
Necrotizing infections are rare but serious.
About 500–1,000 new U.S. cases each year.
Odor often appears before other symptoms.
I’ve seen early recognition prevent life-threatening escalation.
Journal of Surgical Research
Cases are increasing.
NSTIs nearly doubled: ~6,600 in 1999 to ~13,600 in 2007.
Rising alongside diabetes, obesity, and immune disorders.
In my view, odor awareness is more critical than ever.
Oxford Academic
Skin infections create a heavy burden.
SSTIs are a major share of U.S. infectious disease cases.
Diabetic foot infections are especially high risk.
I’ve met patients who ignored odor until it was too late.
Oxford Academic
Final Thought & Opinion
Necrosis odor is a warning.
The smell of necrotic skin tissue—foul, putrid, sometimes sweet—appears early and signals danger.
I’ve seen odor appear first.
In some patients, the smell came before the skin looked severe. Acting fast saved limbs and lives.
Odor is more than unpleasant.
It’s the body’s urgent message that tissue death or infection is underway.
My perspective:
Odor should be treated like pain, fever, or swelling.
Patients, caregivers, and families must learn to recognize it.
Technology matters, but sometimes the nose is the most reliable diagnostic tool.
Necrosis odor is a warning.
The smell of necrotic skin tissue—foul, putrid, sometimes sweet—appears early and signals danger.
I’ve seen odor appear first.
In some patients, the smell came before the skin looked severe. Acting fast saved limbs and lives.
Odor is more than unpleasant.
It’s the body’s urgent message that tissue death or infection is underway.
Odor should be treated like pain, fever, or swelling.
Patients, caregivers, and families must learn to recognize it.
Technology matters, but sometimes the nose is the most reliable diagnostic tool.
Next Steps
Seek care immediately.
Call your doctor or go to urgent care if you notice the odor.
Write down details.
Record when the smell started, how it smells, and changes in the wound.
Do not self-treat.
Avoid scraping, cutting, or covering with creams or powders.
Watch for other symptoms.
Fever, swelling, redness, and pain can mean infection is spreading.
Involve caregivers.
Teach family or staff to recognize necrotic odor early.
Be proactive if at risk.
Diabetics, bedridden patients, or those with poor circulation need regular checks.
Early detection and quick action guided by wound care specialists can prevent necrotic tissue from progressing, protect against severe infection, and significantly improve recovery outcomes.
Seek care immediately.
Call your doctor or go to urgent care if you notice the odor.
Write down details.
Record when the smell started, how it smells, and changes in the wound.
Do not self-treat.
Avoid scraping, cutting, or covering with creams or powders.
Watch for other symptoms.
Fever, swelling, redness, and pain can mean infection is spreading.
Involve caregivers.
Teach family or staff to recognize necrotic odor early.
Be proactive if at risk.
Diabetics, bedridden patients, or those with poor circulation need regular checks.